Unveiling the Truth: Who Really Profits from America’s Complex Healthcare System?

Introduction
The American healthcare system has long been a subject of debate and criticism. With healthcare spending reaching a staggering $4.3 trillion annually, the United States spends more on healthcare than any other developed country. However, despite the high expenditure, American adults have shorter lifespans and higher infant mortality rates compared to other affluent nations. While pharmaceutical companies and hospitals often take the blame for the inflated costs, there is a group of middlemen who extract significant profits from the complexity of the healthcare system. In this article, we will explore who truly profits from America’s baffling healthcare system and the implications of their influence.
The Rise of Big Health
Over the past decade, a small number of intermediaries, known as “big health,” have quietly increased their presence in the American healthcare industry. These intermediaries include insurers, pharmacies, drug distributors, and pharmacy-benefit managers (PBMs). Despite not directly manufacturing drugs or treating patients, these middlemen have become major players in the healthcare market. In 2022, the combined revenue of the nine largest middlemen accounted for around 45% of America’s healthcare bill, a significant increase from 25% in 2013. Big health has even surpassed big tech and big pharma in terms of revenue and market capitalization.
The Oligopoly of Big Health

Big health began as a collection of oligopolies, with a few dominant players controlling significant portions of the healthcare market. Four private health insurers account for 50% of all enrolments, with UnitedHealth Group leading the pack. UnitedHealth made $324 billion in revenues last year, making it one of the most valuable companies in America. Similarly, four pharmacy giants generate 60% of the country’s drug-dispensing revenues, with CVS Health leading the industry. Three PBMs handle 80% of all prescription claims, and three wholesalers control 92% of all drug distribution. These concentrated market shares give big health significant power and influence over the healthcare system.
Vertical Integration and Revenue Channels

To further expand their reach and profitability, the oligopolists have pursued vertical integration into other aspects of the healthcare supply chain. The Affordable Care Act of 2010 placed limits on the profits of health insurers but did not impose similar restrictions on physicians or intermediaries. This created an incentive for insurers to acquire clinics, pharmacies, and other healthcare entities and steer customers toward their subsidiaries. By integrating various components of patient care, big health aims to align incentives and increase overall profitability.
The Benefits and Concerns of Vertical Integration
Proponents of vertical integration argue that consolidating different aspects of patient care under one roof can lead to cost savings and improved coordination. Kaiser Permanente, a role model for integrated care, has historically been praised for its efficiency and high-quality healthcare. However, studies have shown that after hospitals acquire physician practices, prices tend to rise without a significant improvement in the quality of care. Critics also express concerns that vertical integration may limit competition and lead to higher prices for rival providers. Additionally, there are worries about physicians prioritizing cost over quality when they are part of the same business entity.
The Profitability of Big Health
One notable aspect of big health is its extraordinary profitability. Research has found that intermediaries in the healthcare supply chain earn higher annualized excess returns compared to the S&P 500 as a whole. Between 2013 and 2018, these intermediaries enjoyed an annualized excess return of 5.9%, while the S&P 500 averaged 3.6%. This profitability has attracted the attention of newcomers who aim to disrupt the market. Upstart health insurers and innovative pharmacy models, such as Amazon’s foray into healthcare, pose potential challenges to the established players in big health.
Challenges Faced by Newcomers
While newcomers may bring fresh ideas and approaches to the healthcare industry, they face several obstacles. The complexity and long-standing networks of the entrenched firms make it difficult for new players to replicate their success. Building relationships with doctors, hospitals, insurers, and drugmakers takes time and institutional knowledge. Furthermore, the profit limits imposed on insurers by the Affordable Care Act pose challenges for upstarts in the insurance business, as they struggle to compete against the negotiating power of integrated giants. Despite the challenges, newcomers like Amazon continue to expand their healthcare businesses and explore innovative solutions.
Regulation and Oversight of Intermediaries
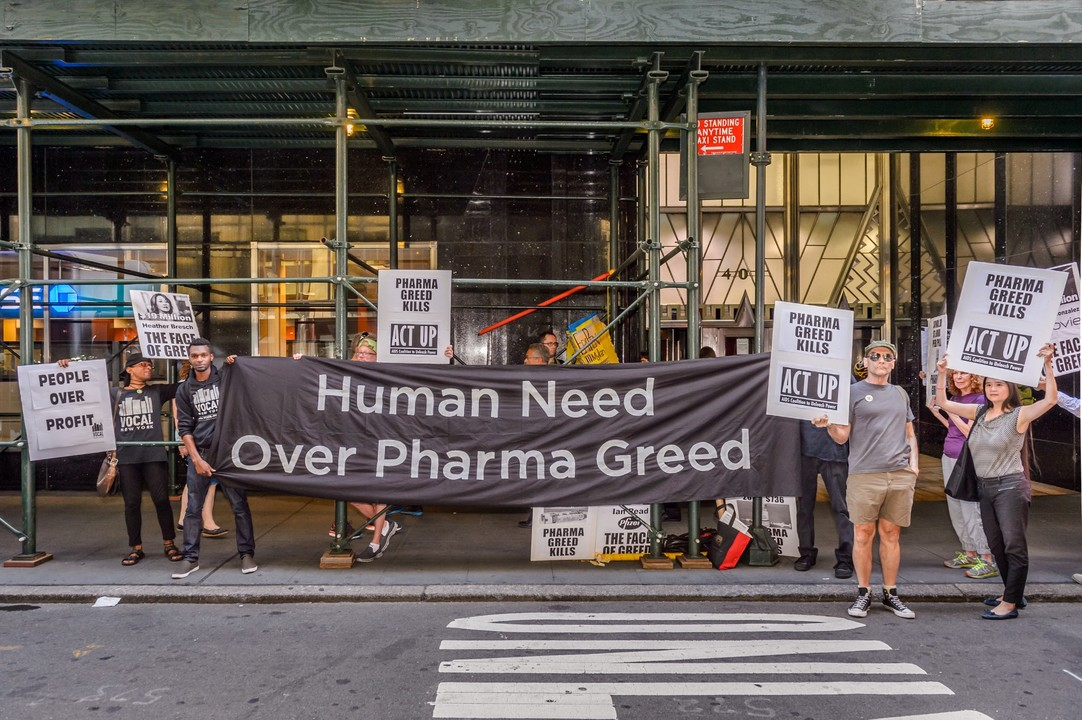
The role of intermediaries in the healthcare system has not gone unnoticed by regulators and lawmakers. Pharmacy-benefit managers, in particular, have faced scrutiny for their opaque pricing practices and potential anticompetitive behavior. Several bills are currently under consideration in Congress to regulate PBMs and increase transparency in drug pricing. The Federal Trade Commission (FTC) has also launched investigations into the business practices of major PBMs. These regulatory efforts aim to address the concerns raised by critics and ensure a fair and competitive healthcare market.
The Future of America’s Healthcare System
The influence of big health on America’s healthcare system is undeniable. As the industry continues to evolve, it remains to be seen whether the dominance of these intermediaries will persist or if newcomers will disrupt the status quo. The ongoing debates about healthcare reform, drug pricing, and access to care will shape the future of healthcare in the United States. Ultimately, the goal should be to create a system that prioritizes affordability, quality, and equitable access for all Americans.
Conclusion
America’s complex healthcare system involves a wide range of players, including insurers, pharmacies, PBMs, and wholesalers. These intermediaries, collectively known as big health, extract significant profits from the system’s complexity. While vertical integration and consolidation may bring some benefits, concerns about market concentration and potential anticompetitive behavior persist. The profitability of big health has attracted newcomers eager to disrupt the industry, but they face significant challenges in establishing themselves. Regulation and oversight are crucial in ensuring a fair and transparent healthcare market. As the healthcare landscape continues to evolve, it is vital to prioritize affordability, quality, and accessibility for all Americans.
